“Dysfunctional” is the verdict on the Dhulwa Secure Mental Health Unit, the ACT low to medium security facility for people involved with the criminal justice system, according to an independent report commissioned by the ACT Government and tabled yesterday by Emma Davidson, minister for mental health.
The report was announced in May, following complaints by the Australian Nursing and Midwifery Association (ANMF) ACT Branch that Dhulwa may well be the worst mental health facility in the country – complaints the ACT Government and Canberra Health Services tried to play down at the time.
Nurses reported 100 physical assaults by patients, including for 13 days in a row in February; nurses could not provide proper care for unwell patients due to government failings; and the work culture was “rotten”, Matthew Daniel, secretary of the ANMF ACT, stated earlier this year. WorkSafe ACT issued a prohibition and improvement notice over one incident the same week a nurse was maimed in another incident. One nurse likened working there to being “sent into the killing fields”.
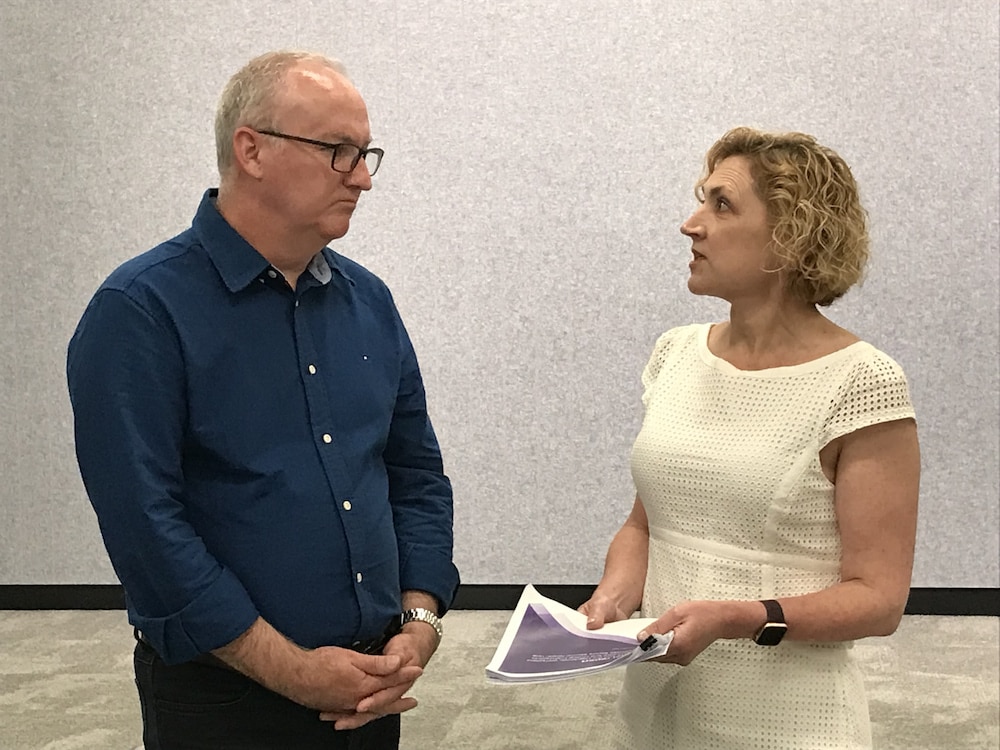
Ms Davidson described the report as “really hard reading” and “confronting”. But both the ACT government and the ANMF hope that the report will solve the problems at the troubled facility.
“If we have the courage to really listen when people are telling us these really difficult things, that’s when we can find ways to make things better,” the minister said.
“This report will go a long way to fixing the problems,” Mr Daniel said. “We need them fixed. We can’t be standing again here in a couple of years’ time.”
- Inquiry at Dhulwa facility needed, nurses’ union says (6 April)
- Danger and desperation at Dhulwa Mental Health Unit (7 April)
- Dhulwa management has acted swiftly, CHS says (7 April)
- ANMF claims Dhulwa nurses unable to provide proper care (8 April)
- Nurses repeat call for inquiry into work safety at Dhulwa (20 April)
- ACT government finally agrees to Dhulwa Mental Health Unit inquiry (2 May)
- Chair appointed to Dhulwa inquiry, reference terms revealed (31 May)
The report finds that “complex and unsettled governance arrangements at Dhulwa likely precipitated significant and concerning workplace safety and clinical practice matters”.
The Model of Care was unclear. Lack of consistent leadership, effective consultation, and clear communication led to a poor work culture. Uncertainty about safety arrangements contributed to safety concerns. WHS practices were reactive. WHS and clinical governance did not take a best practice approach to risk management. The review of incidents could be improved. Approaches to understanding aggression were inconsistently understood and applied. The Dhulwa workforce did not have the support, training, and development to manage the complexity of patients. Safety at Dhulwa could be improved by the introduction of Safewards, a program that encourages staff and clients to work together, and trauma-informed care.
Submissions highlighted the dysfunction between different levels of the workforce, the report stated: unsupportive leadership; poorly managed change; fractured workforce relationships; poor communication and lack of transparency; and workforce cliques.
Over the period of the inquiry, the report noted, Canberra Health Services and the Dhulwa leadership team had worked to improve practices and procedures; introduced and evaluated daily ‘safety huddles’ during shift changes to identify any potential issues that may threaten staff or patients; recruited to fill vacancies in nursing leadership roles; trained nursing staff; and trained all staff in preventing and managing aggression to reduce occupational violence risks (completed by 95 per cent of staff). A Clinical Nurse Educator has been recruited to structure and facilitate team education programs and reinvigorate the Safewards model in Dhulwa. A new assessment tool called Dynamic ISBAR (Introduction, Situation, Background, Assessment, Recommendations/Read back) has been introduced.
The report stated that Dhulwa could have been highly successful: it was purpose-built, provided with the best training, policies, and procedures of the time, and well resourced. But Canberra Health Services and the Dhulwa workforce failed to take full advantage of the opportunities provided, the report stated. “The standard of care at times … is well below that expected of the unit and contemporary practice.”
The ANMF had been concerned about governance for a long time, Mr Daniel said; policies and procedures did not match, or were changed on the fly, while care was being delivered; and staff did not know what the model of care was.
“You can’t operate safely in that sort of environment,” Mr Daniel said.
The inquiry makes 25 recommendations for the ACT Government to consider, focusing on clinical care and service delivery, work health and safety, workplace relations, governance, leadership, culture, and engagement. These are similar to findings and recommendations made by previous reports – which did not lead to significant or lasting improvements, the report noted.
“There has been a level of dysfunction occurring at Dhulwa for some time, and the implementation of the Inquiry recommendations will require a commitment to change and an investment of both time and resourcing if improvements are to be made,” the report stated.
Ms Davidson would not say whether she accepted all the recommendations – they required a formal response from the government – but she would work with the ANMF ACT and Canberra Health Services to implement them.
The first recommendation is for independent oversight of the implementation of the recommendations to ensure that change occurs at Dhulwa, and that the change is effected as soon as reasonably practicable. Ms Davidson considers this a priority; the government is already discussing with the ANMF and Canberra Health Services what criteria to look for and what skills are needed.
Many recommendations can be implemented quickly, Ms Davidson said, because they relate to how care is provided and staff supported. There was no reason why some could not be put in place immediately, before the government’s formal response, she thought.
Mr Daniel believes the ANMF will be able to support all 25 recommendations.
“They’re solid; they go to the heart of the issues our members raised,” he said.
Mr Daniel noted there had been “attempts to move forward” on some issues raised, although some about the Dhulwa management were sticking points for the ANMF. He believes these can be addressed.
Staffing remains difficult, Mr Daniel said: unregulated workers are filling gaps where there are no registered nurses, while registered nurses are being brought in under agency arrangements – a stopgap measure; he believes the government must make sure full staffing is always maintained.
The inquiry was meant to provide the report within 18 weeks; the report was received on 11 November, and tabled yesterday, 1 December, on the last sitting day of the year. Ms Davidson denied the government had sat on the report. The inquiry was under the Inquiries Act 1991, and handled through the Chief Minister’s office, showing its importance, Ms Davidson said.
Canberra Daily is keen to hear from you about a story idea in the Canberra and surrounding region. Click here to submit a news tip.