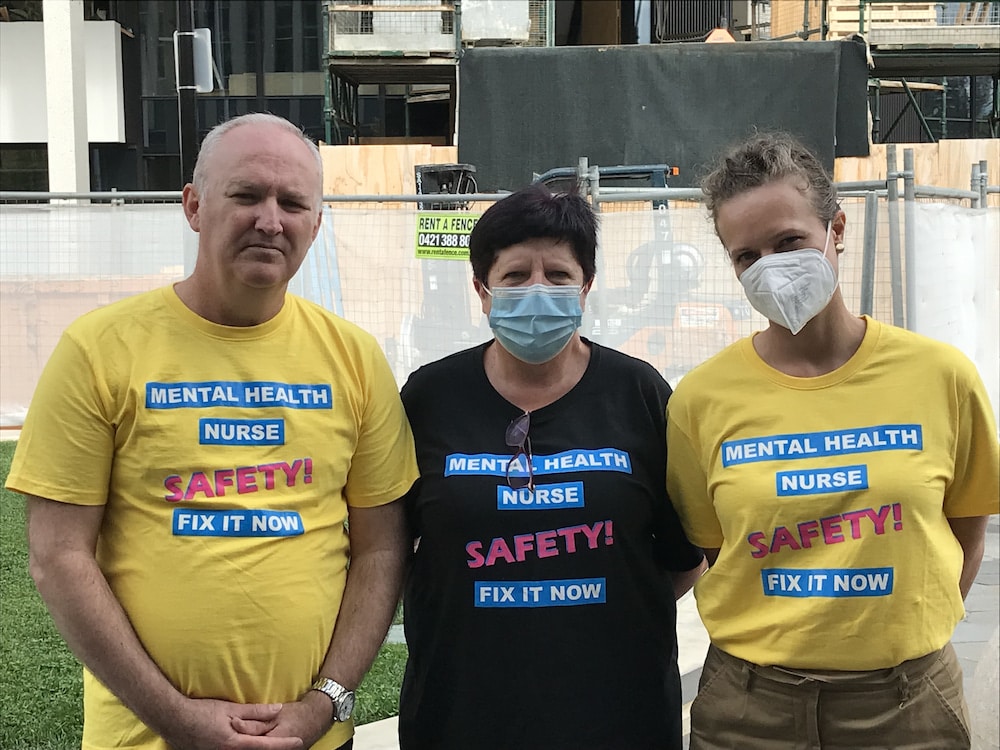
Nurses at the Dhulwa Mental Health Unit, the ACT low to medium security facility for people involved with the criminal justice system, say it may well be the worst mental health facility in the country, according to their union – and the ANMF is urgently calling for a government inquiry before someone is killed. And if the government does not act, the union may take industrial action.
Nurses reported 100 physical assaults by patients over the six months to February, stated Matthew Daniel, branch secretary of the Australian Nursing and Midwifery Association (ANMF) ACT Branch.
Nurses suffered broken arms, broken noses, and broken fingers, Mr Daniel said; others had faeces and urine thrown at them. Patients beat up other patients; often the attacks were racially motivated.
Patients assaulted nurses for almost 13 days in a row in February, Mr Daniel said. On 31 January, one ‘consumer’ (patient) assaulted another; on 1 February, staff were physically assaulted; on 3 February, many staff were assaulted; on 5 February, again, many staff were assaulted; and assaults continued on 6, 8, 9, 10, 11, and 13 February.
Working there, one nurse told Mr Daniel, was like being “sent into the killing fields”.
Canberra Health Services has downplayed the level of violence, claiming that the majority of the 83 incidents happened within the last month or so, due to “specific circumstances” at the unit.
Karen Grace, CHS executive director of nursing and midwifery, said the executive responded immediately, as soon as the incidents started to occur.
They increased resourcing for the unit, and rostered senior mental health clinicians in leadership roles across the service to ensure staff had support on the ground from very experienced mental health nurses, including a director of nursing. An assistant director of nursing, a former mental health nurse at Dhulwa, is reviewing the occupational violence strategies.
“We’re doing absolutely everything we can to mitigate the likelihood of a recurrence,” Ms Grace said.
Last month, the ANMF twice met Emma Davidson, ACT Minister for Mental Health, and, in Mr Daniel’s words, “pleaded” with her for the government to conduct an inquiry.
“We have days to address this, not weeks,” Mr Daniel said he told Ms Davidson.
“We want to look at all of the practices and policies such as the admission criteria, adherence to policies, review of policies, and the complete operations of staffing levels, the management practices, the HR practices to really review what’s going on from both a nurse perspective and patient perspective,” Mr Daniel told Canberra Daily.
Nurses told Ms Davidson that some found it difficult to get out of bed and go to work because they were stressed and fearful of what might happen to them, Mr Daniel told CW. Many are looking for jobs elsewhere, he said – but not with CHS.
“By the sheer volume of assaults, they’ve shown they’re unable to deal with the problem,” Mr Daniel said.
ACT Government response
At a press conference today, Ms Davidson did not announce an inquiry, but said she had listened to the nurses’ concerns.
Canberra Health Services was working with nurses at Dhulwa to address procedures and “what’s been happening in that workplace quite extensively”, Ms Davidson said.
“We want to work with these nurses and with their representatives to make sure that their concerns are being listened to, that they are being understood, and that we can work with them to make improvements to their workplace and make it safe,” she said.
“It’s really important for everyone to have a safe and healthy workplace, and to know that when you go to work, that you’ll feel safe, and that you will be supported.”
Over the last few years, Ms Davidson said, the government had embarked on cultural reform and workplace safety across the ACT – including at Dhulwa.
Violence in mental health facilities had reduced over the last couple of years, she stated, and February’s events were exceptional, “due to some very specific circumstances”, such as workforce pressures across the entire health service due to COVID-19.
“When you have large numbers of your workforce who are out on quarantine, or who are experiencing a lot of pressure, that does have an impact on your shift rosters,” Ms Davidson said.
“I understand that those incidents are no longer occurring at that kind of rate.
“It’s not something that I would expect to see ongoing.”
ANMF is disappointed
The government response left Mr Daniel unimpressed.
“It’s clear … that they just do not have the answers,” he said. “For the Minister and the government to come out and say that they’ve been putting in solutions to the problems just isn’t borne out by the evidence. Why do we have so many incidents of occupational violence?”
Nor, Mr Daniel said, did he accept the Government’s narrative that the problem was restricted to February; the assaults had occurred for six months at least. (The ANMF also protested about the issue in 2018; violence at Dhulwa came in peaks and troughs.)
“We’re going to be on the government’s back to come up with an inquiry,” Mr Daniel said. “Nothing less will do. So we will continue to talk with the government about an inquiry, and they need to deliver for our members. They need to make sure that nurses are kept safe.”
“The number of assaults cannot continue,” Mr Daniel told CW earlier today. “Every day that we wait for an outcome, some sort of intervention by the government, is another day where a nurse is at risk or is actually being assaulted.
“What worries our members is they know one punch can kill. … It only takes one particular assault for a nurse to be knocked unconscious, hit their head on the floor, and it could be devastating. There’s plenty of cases where that’s occurred in other jurisdictions, where nurses haven’t been protected from this level of violence. I would hate for it go to a coroner’s inquiry, and for a coroner to come back with the findings that a death could have been avoided.”
Industrial action is on the table, Mr Daniel said; while Dhulwa is dangerous, the ACT’s nurses and midwives complain of being overworked and understaffed.
“Our nurses and midwives are asking us when they can strike, when they can go out. They’re sick of the understaffing, which occurred way before COVID. And they need the government to take action to relieve the pressure. We don’t see a recovery plan. We don’t see any immediate relief. They’re talking about opening beds, opening theatres, opening ICU beds. There’s no staff.”
To their credit, Mr Daniel said, the ACT Government plans to recruit 400 more nurses and midwives by 2024 to address the ratio problem. “But that is not going to provide the solution in the next six months.”
Leanne Castley MLA (Canberra Liberals), Shadow Health Minister, also called on Ms Davidson to announce an independent review.
“This is a serious situation the government cannot ignore,” Ms Castley said. “I am particularly concerned at the damning comments by the ANMF who say the ACT Government is ignoring their safety and workload concerns.”
More to follow.