Emergency! The ACT’s hospital emergency department waiting times are some of the longest in the country, for the fifth year in a row, according to the 2021–22 Report on Government Services published last week.
The ACT Government blames COVID-19, influenza, and deferred care, and says it is committed to improving wait times – but the Canberra Liberals say the public are tired of excuses for the “abysmal” performance.
ROGS: Long wait times
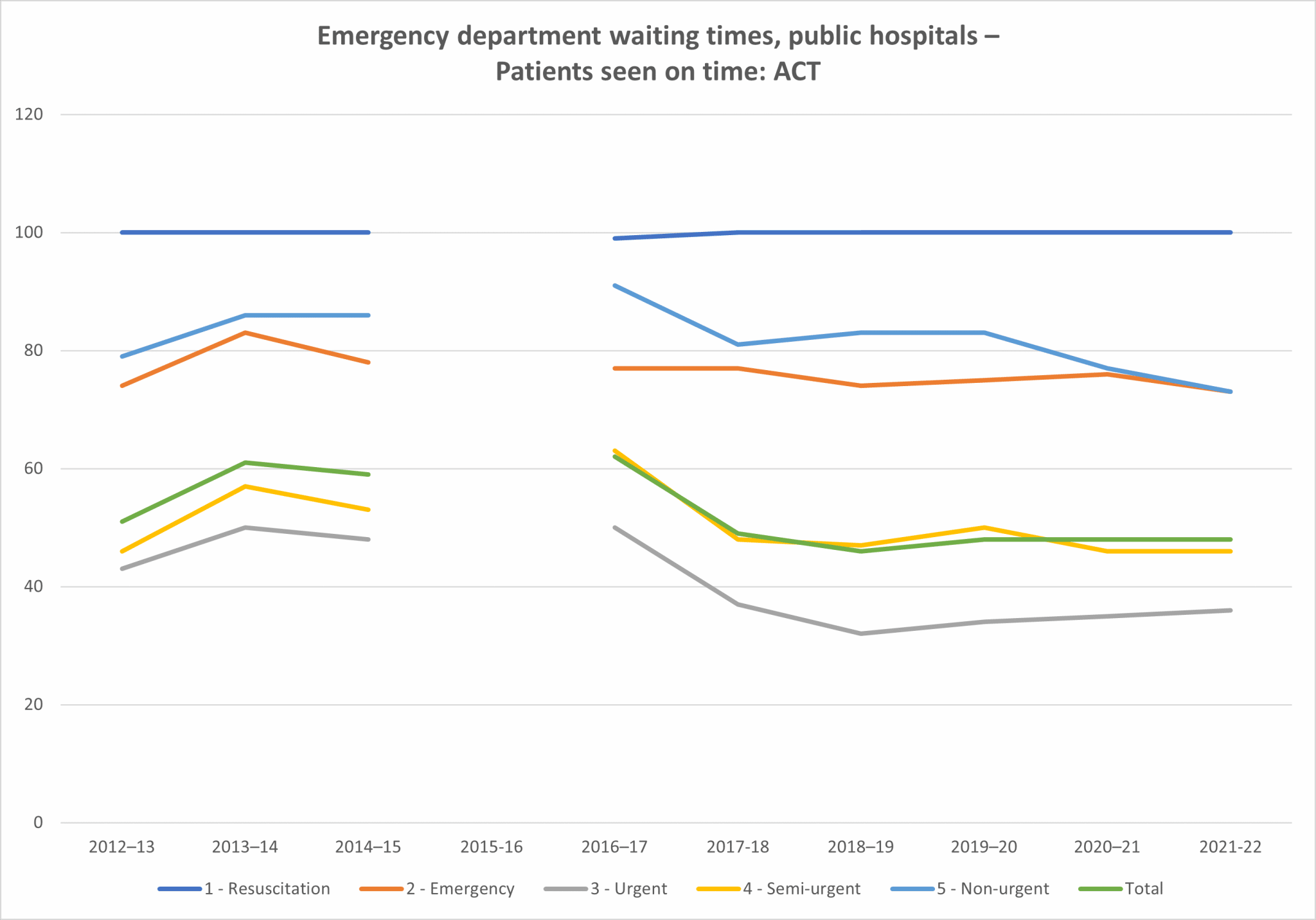
The data shows that the ACT saw less than half (48 per cent) of emergency department patients on time for the fifth year in a row (since 2017-18).
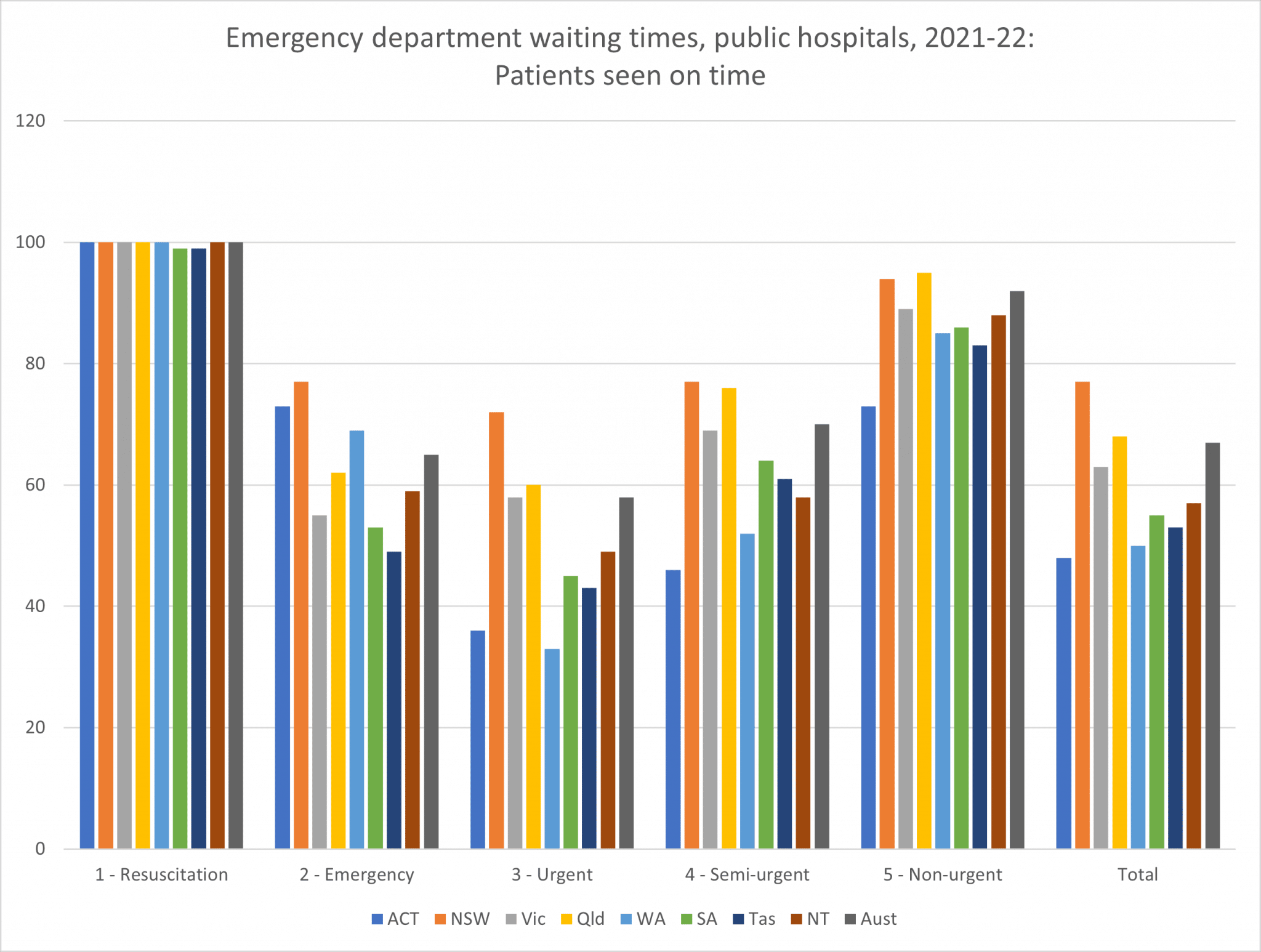
The ACT is the second best in the country for seeing emergency (category 2) patients on time (73 per cent, above the national average of 65 per cent), and 100 per cent of resuscitation (category 1) patients are seen on time.
“This means for the most time-critical presentations, Canberrans receive some of the most timely treatment in Australia,” health minister Rachel Stephen-Smith said.
But the ACT has the second worst waiting times for seeing urgent (category 3) patients (36 per cent, 22 points below the national average of 58 per cent) on time, and the worst for seeing:
- semi-urgent (category 4) (46 per cent, 24 points below the national average of 70 per cent),
- non-urgent (category 5) (73 per cent, 19 points below the national average of 92 per cent).
The ACT has the longest total waiting times (48 per cent, 19 points below the national average of 67 per cent).
The proportion of patients seen on time is decreasing. The proportion of emergency patients seen on time in 2021–22 (73 per cent) is 10 per cent less than in 2013–14 (83 per cent). The proportion of semi-urgent patients seen on time has also fallen, from 63 per cent in 2016–17 to 48 per cent in 2017–18, stabilising at 46 per cent in 2020–21 and 2021–22. As a result, the total number of patients seen on time slipped from 62 per cent in 2016–17 to 48 per cent for the last three years.
Five years ago, 91 per cent of non-urgent patients were seen on time; in 2021–22, only 73 per cent were.
The proportion of urgent patients seen on time (58 per cent), however, is recovering from a fall in 2017–18, although still well below 2016–17 figures.
Ms Stephen-Smith stated that the Delta and Omicron waves of COVID-19, an early and significant influenza season, and the impacts of deferred care challenged the ACT’s hospitals and urgent care services, like all health systems across the country, throughout 2021-22.
“This affected performance across the system due to the availability of workforce and increased complexity in supporting hospital presentations,” Ms Stephen-Smith said.
Elective surgery waiting lists expanded significantly due to COVID-19, both in the ACT and across Australia, Ms Stephen-Smith noted.
“Through early planning and response in 2020-21, the ACT Government has tried to minimise the impact, and has invested additional funds throughout 2021-22.”
The ACT Government will invest $2.6 billion across the health portfolio this year to procure more frontline health workers, new state-of-the-art facilities, and better care in the community, a spokesman said in December. The 2021–22 Budget included $23 million to boost Canberra Hospital’s emergency department, while the 2022–23 Budget included $17 million to buy more intensive care unit and in-patient beds at Calvary.
- ACT mixed results for ED waiting times and elective surgeries (7 December 2022)
“Across the other triage categories, there is still work to do to improve patient flow across the hospitals and enable the Emergency Departments to operate more efficiently,” Ms Stephen-Smith acknowledged. “This is why the ACT Government continues to deliver record levels of investment to drive improvements and reduce pressure across the system.”
Ms Stephen-Smith emphasised more positive trends. In 2021-22, 15,831 patients were added to public hospital elective surgery waiting lists, and 16,644 people were removed from the waiting list.
“It is encouraging that our efforts to date are paying off in regard to elective surgery,” Ms Stephen-Smith said. “The ACT is the only jurisdiction that has consistently been able to remove more patients from the elective surgery waiting list than have been added to it each year for the last five years.”
The ACT is unique in having two public hospital emergency departments servicing both the ACT and surrounding NSW populations, Ms Stephen-Smith noted.
When compared against peer hospitals across Australia for percentage of patients seen on time in the emergency department in 2021-22, Canberra Hospital (a Public principal referral hospital) performed better (48 per cent) than its peers in Tasmania (38 per cent), South Australia (40 per cent), and Western Australia and the Northern Territory (46 per cent), Ms Stephen-Smith remarked.
However, it performed 27 points below NSW (75 per cent), 24 points below Queensland (72 per cent), 14 points below Victoria (62 per cent), and 16 points below the national average.

Calvary (as a Public acute group A hospital) also performs better (49 per cent) than the averages of peer hospitals in Western Australia (37 per cent) and South Australia (41 per cent), Ms Stephen-Smith observed.
Nevertheless, Calvary performed 26 points below NSW (75 per cent), 17 points below the Northern Territory (66 per cent), 14 points below Victoria and the national average (63 per cent), 13 points below Queensland (62 per cent), 10 points below Tasmania (59 per cent).

Canberra Liberals
Leanne Castley MLA, Shadow Minister for Health, described the statistics as “abysmal”.
“Canberrans are demanding better healthcare from the Labor-Greens government,” Ms Castley said.
“Every year the Barr-Rattenbury government has managed the health system, it has performed worse than the national average.
“It is embarrassing and, more importantly, having a real impact on Canberrans’ health outcomes.
“Each year, we hear new excuses from the Health Minister about what she is doing to fix this crisis.
“After a decade below the national average and no improvement, Canberrans are tired of excuses and spin from this government.
“Last week, a grandmother contacted my office on behalf of her eight-year-old granddaughter, who waited in pain following a surgical complication for more than six hours before being seen by a doctor at the emergency department.
“Canberra families deserve access to timely care when their loved ones have to use the public health system.
“How can the government justify 3 billion dollars for a tram extension when the statistics tell us that the ACT’s health system is in perpetual crisis?”
ACT Government response
The Canberra Hospital and Calvary Public Hospital Bruce were absolutely committed to improving emergency department, elective surgery, and outpatient wait times and waiting lists, Ms Stephen-Smith said. Only a whole of system approach will improve wait times, she believes.
“Our hospitals are identifying ways to improve efficiencies, patient flow, and patient discharge.”
Canberra Health Services trialled several new innovative models of care, the minister said.
The ACT Government invested $22.9 million through the 2021-22 Budget to fund new programs and models of care at the Canberra Hospital. The Emergency Medical Unit at Canberra Hospital was expanded to 18 spaces, and a medical navigator and a new Acute Medical Unit were introduced to facilitate admissions as quickly as possible.
The ACT Government has a three-year, $30 million plan funded through the 2022-23 Budget to meet its target of 60,000 elective surgeries by 2024–25, building on the “excellent” work of the Territory-wide surgical services team and private partners, Ms Stephen-Smith said.
Ms Stephen-Smith believes the federal government must provide more funding for healthcare.
“Across the country, there is a need for more investment in primary care and significant improvements to aged care, both of which are Commonwealth responsibilities,” she said.
“Providing more care in the community at an earlier stage of someone’s illness can prevent a person needing to present to the emergency department or be admitted into hospital. The ACT Government will continue to work with the Commonwealth Government to improve primary care and ensure every Canberran has access to the right healthcare, at the right time.
“States and Territories also continue to advocate for improvements in the way the Commonwealth contributes to hospital funding, including removing the growth cap and moving towards 50:50 funding.”



