Following considerable public pressure over the past few weeks, the federal government has announced concession card holders will soon be able to collect up to ten free rapid antigen tests over three months.
But everyone else will continue to have to purchase their own rapid antigen tests, which cost upwards of A$10 a test.
In countries like Singapore, the UK and Germany, rapid antigen tests are free for everyone.
We’ve developed a model that estimates how cost-effective a policy of government-funded rapid antigen tests for all Australians would be. We’ve released our economic analysis as a pre-print online, which is yet to be independently reviewed by other researchers.
We found a policy of government-funded rapid antigen tests for all is highly likely to be cost-effective.
Even minor reductions in COVID transmission rates due to increased early isolation would justify the additional costs associated with the policy.
Here’s why.
Why is testing so important?
Testing and contact tracing have been the primary measures used to interrupt the spread of COVID around the world.
One of the benefits of testing for cases is it allows countries to rapidly identify new cases, isolate affected people and their close contacts, and thereby slow further transmission of the disease.
Australia has relied on PCR (polymerase chain reaction) tests to confirm COVID cases, which are funded by the federal government and free for Australians.
But the emergence of the highly transmissible Omicron variant, coinciding with a relaxation of public health restrictions and the social festive season, has led to a surge in COVID cases in Australia, swamping the PCR testing system.
Governments are pivoting towards using rapid antigen tests to confirm positive cases, which can give results in 15 minutes, although they’re not as accurate as PCR tests.
How does our analysis work?
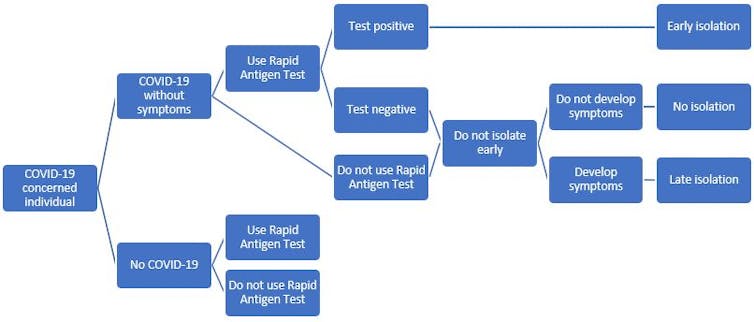
We created a “decision tree” model, which represents the testing pathways for a hypothetical group of people without COVID symptoms.
We used it to estimate the number of COVID-positive people isolating before developing symptoms.
It’s key people isolate as early as possible, to reduce the risk of spread to others.
We analysed a range of possible scenarios.
A key parameter is the proportion of people who use a rapid antigen test who have COVID.
Let’s play out one scenario.
Let’s say a group of 10,000 people get free rapid antigen tests funded by the government. Assume 1,000 out of 10,000 users have COVID, and that a rapid antigen test costs $10.
Let’s also assume 2,000 of the 10,000 would buy rapid antigen tests if not government-funded. (The real-life proportion who would be willing and able to buy a rapid antigen test is impossible to know, given the current shortage.)
What did we find?
In the group where everyone had access to free rapid antigen tests, the model estimates this policy would result in successfully isolating an additional 464 people early, compared with a group in which 20% purchased their own rapid antigen tests.
Providing free rapid tests for 10,000 people would cost the government $100,000, but spending less on PCR tests (which are about $150 each) reduces the additional costs to the government to around $52,000.
Rapid antigen tests are less effective in people with no symptoms, so they wouldn’t catch everybody in the group who’s COVID-positive.
But the net effect is preventing an additional 464 people from infecting more people, thereby reducing costs to the economy of further infections. The costs of these people isolating only after developing symptoms would likely be far higher than the extra $52,000 spent on tests.
Dividing the $52,000 by the 464 earlier isolating cases gives us an estimate of the cost to the government per additional earlier isolating person with COVID – $112. This allows us to compare alternative scenarios.
For example, if only 500 of 10,000 users of government-funded rapid antigen tests had COVID, 232 more people would isolate early and the cost per additional earlier isolating person with COVID would be $328.
If only 100 of 10,000 users have COVID, the corresponding value is $2,052.
The less COVID circulating, the less effective a policy of free rapid antigen tests for all would be. But even with low prevalence, it’s still highly likely to be cost-effective.
The expected benefits of early isolation are difficult to quantify, but it can only help to constrain the spread of COVID and the number of people infected by each person with COVID (the reproductive number). Modelling shows that in Australia the reproductive number increased from around 1 to 1.5 over the course of December 2021, and daily reported COVID cases increased from around 1,000 to over 30,000. This illustrates the importance of the reproductive number and the magnitude of the potential effects of increasing early isolation of people with COVID. Even a minor reduction in the reproductive number will have a significant effect on the number of daily cases.
There are high costs to health and the economy of not successfully isolating COVID positive people early.
COVID positive people, who don’t know they’re positive, will spread it to others, many of whom will get sick, require medical attention, and take time off work. Some will need to go to hospital, be in intensive care, and be put on a ventilator. And some will die.
A proportion of those who do recover from the initial phase of the infection will have lingering symptoms from the virus, known as “long COVID”.
All of these outcomes impose significant costs to people and society. We could make a conservative assumption that each early isolated case prevents at least one new COVID case and that the broad range of costs associated with one COVID case are far higher than the $112 it might cost the government per additional early isolated person with COVID.
Are there any downsides?
One thing to consider is overuse. If people used rapid antigen tests too much, for example when people are highly unlikely to have been exposed to COVID, this would reduce the cost-effectiveness of the policy.
In saying that, the unpleasant nature of the testing process should limit such overuse – no one enjoys sticking the swab up their nose!
Hoarding is another risk, as with toilet paper in the early days of the pandemic. So it would be important to ensure confidence in the supply and distribution of the tests.
Constraining the spread of COVID is important for many reasons, including avoiding short- and long-term health effects, reducing burden on the health system, and increasing availability of essential workers.
Easy and equitable access to testing is a cornerstone of the public health response to COVID. It also makes economic sense.
Jonathan Karnon, Professor of Health Economics, Flinders University; Billie Bonevski, Professor of Public Health, Flinders University, and Hossein Haji Ali Afzali, Associate Professor in Health Economics, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Get all the latest Canberra news, sport, entertainment, lifestyle, competitions and more delivered straight to your inbox with the Canberra Daily Daily Newsletter. Sign up here.



