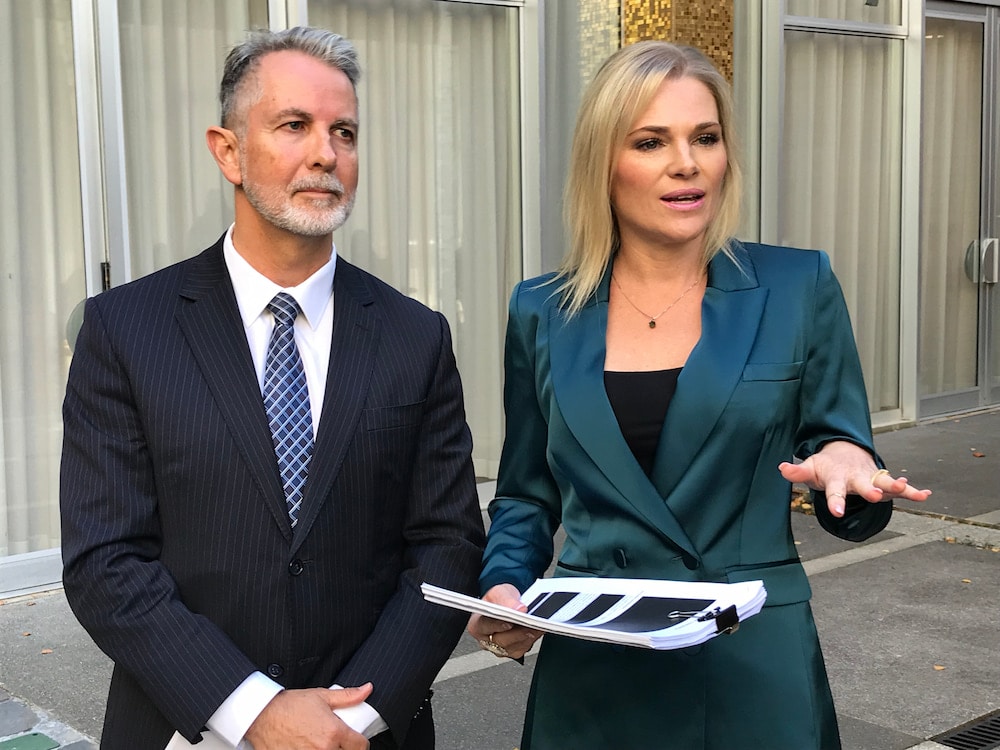
The Canberra Liberals claim that the ACT’s health system is “broken” and have called for a Royal Commission to investigate its failures, current needs and future requirements. The acting opposition leader, Jeremy Hanson MLA, will introduce a bill in the Legislative Assembly next week.
“It’s a system that is in crisis,” Mr Hanson said. “It needs a long-term fix. The way that can happen is through a Royal Commission.”
The Liberals intend that the Royal Commission would look at all areas of the ACT Health System, including the governance, organisation structures, resourcing and effectiveness of Canberra Health Services, ACT Health, Calvary Hospital, and the Local Hospital Network.
Royal Commissions have been conducted into aged care, veterans’ affairs, and banking federally, and into the mental health service in Victoria, Mr Hanson noted.
Health minister Rachel Stephen-Smith MLA, however, does not think a Royal Commission is necessary.
“We understand what the problems are, and what we need to do is implement the plans that we have to address the challenges that we face,” she said. “The Canberra Liberals’ announcement today is simply an indication that they don’t have any plans to do anything differently.”
Problems with the health system
The Canberra Liberals can back up their claim with a long list of problems.
This week, the AMA’s report card found that “the ACT public hospital performance sits disappointingly below the expected standard on measures that are considered to be important to consumers and the quality of healthcare”. Nationally, for instance, the ACT was the worst performer for emergency department (ED) visits completed in four hours or less, while the ACT was below the national average on wait times for planned surgery. Earlier this year, the Report on Government Services (ROGS) also stated that the ACT had the longest ED wait times in Australia.
- ACT has longest ED waiting times in country: ROGS (6 February)
There are thousands of people on surgery waitlists, the Liberals say: elective surgery patients wait years on hidden waiting lists to see specialists in hospital outpatient clinics, while more than 6,000 patients are overdue for endoscopy.
Frontline staff are at breaking point due to a poor workplace culture, the Liberals say. Nurses and midwives told last year’s Inquiry into a Recovery Plan for Nursing and Midwifery Workers they were “burned out, drained, angry, disheartened, exhausted, fed up”, shadow health minister Leanne Castley said.
A 2021 workplace culture review showed that 23 per cent of nurses and medical officers were bullied, and one in eight nurses and one in four medical officers intended to leave. An ANMF survey stated that the culture at Canberra Health Services was the worst it had ever been, while nurses and midwives complained of lack of proper workforce planning; chronic staff shortages, skill-mix issues, and excessive overtime; burnout, stress, fatigue, and poor psychosocial wellbeing; and worsening workplace culture, including poor morale.
Cardiologists say the health system is ‘parlous’ due to poor managerial decisions made by senior members of ACT Health directorate.
Last month, Worksafe ACT issued two notices to Canberra Hospital’s Intensive Care Unit (ICU) for fatigue management and risks.
The Fetal Medicine Unit lost its training accreditation last year.
- Calls for transparency over Canberra Fetal Medicine Unit training (29 March)
- CPSU: CHS has ‘dropped the ball’ on Fetal Medicine Unit (20 April)
- CHS: Outsourcing Fetal Medicine Unit jobs is ‘simply untrue’ (21 April)
Canberra has the most expensive doctors, the lowest bulk billing rate, and the highest average out of pocket costs in the country, according to the Cleanbill Health of the Nation Report, the first comprehensive survey of GP clinic availabilities and billing practices, published last month – and GPs fear that if the ACT Government introduces a payroll tax, they will be forced to increase their bills further or close their clinics.
- Price hike for Canberra doctors on the cards (20 April)
“Day after day, we are bombarded with stories about families with issues with the health system, and the concerns that nurses have,” Ms Castley said.
Some of those stories: A man waited six and a half years for his colonoscopy. A woman waited more than 700 days for her hernia operation. A woman having a miscarriage asked Facebook whether she should go to Sydney. A man waiting for a neurology appointment told Ms Castley it was unlikely he would be seen in his lifetime because he was a category 3 (non-urgent) patient.
“There’s story after story of Canberrans unable to get the health care that they deserve, that they need, here in Canberra,” Ms Castley said. “These things shouldn’t be happening. These are our family members. These are local Canberrans that need help.”
The Canberra Liberals claim that the health system is in decline because the ACT Government diverted money from the hospital to pay for the tram. They allege that real health expenditure was cut by 3.6 per cent per person between 2015-16 and 2018-19.
ACT Government: Royal Commission not needed
Health minister Rachel Stephen-Smith acknowledged there were “significant challenges” in the ACT health system. So, she said, did the rest of the country, and the world. COVID-19, she said, placed pressure on the health system, impacting patients and staff.
But a Royal Commission would be expensive and take time.
“These challenges exist now,” the minister said. “The ACT Government is acting now. We’ve got the plans and strategies in place, and we are already starting to implement those.”
Today, the ACT Government published its 10-year ACT Health Workforce Strategy 2022–23 to attract and retain talented students and recruit and retain new and experienced health care workers.
Ms Stephen-Smith said the Strategy takes a holistic approach, looking across the entire health system – including public health services, primary care, private health, and non-government organisations.
The Strategy identifies eight priority areas to target workforce needs.
“From creating exciting career paths and investing in data intelligence, to ensuring we provide a culturally safe environment for our Aboriginal and Torres Strait Islander workforce, these priorities will help us deliver on our collective ambition to be the most capable health workforce in Australia,” Ms Stephen-Smith said.
She said the ACT Government is ready to begin, or is already working on, 23 actions. Some of the measures have already been introduced: an $8.5 million wellbeing fund (three initiatives implemented) and a $3 million new rostering system to ensure staff in high-pressure areas get the break they need, Ms Stephen-Smith said. The government is considering partnerships with universities that teach courses not offered in the ACT.
- $8.75 million wellbeing fund for ACT public health workers (5 October 2022)
- Wellbeing initiatives to support ACT’s health workforce (6 December 2022)
In Mr Hanson’s view, the strategy “pastes over the fact that [the Third Independent Annual Review 2023 of culture in the ACT public health system] found there is no long-term vision in health when it comes to workforce planning”. Ms Stephen-Smith had said that the government was developing dashboards to understand rates of attrition and occupational violence, and employment types; previously, there was no data.
Last year, too, the ACT Government released its ACT Health Services Plan 2022–30, setting out priorities for government-funded health services over the next eight years:
“A whole of system strategy … right from our universities through our private system through our public health system,” Ms Stephen-Smith said.
- ACT government releases health plan for 2020s (9 August 2022)
“These are big picture strategies with very specific implementation and actions,” the minister said.
“It’s very difficult to see how a Royal Commission could take a broader approach than we have in developing our health services plan that we released last year.”
Nor, Ms Stephen-Smith argued, was a Royal Commission likely to reveal much that was new. Royal Commissions were a useful vehicle for truth-telling, when there was little transparency. But, she maintained, there was a lot of transparency in the ACT.
“We understand what those challenges are. We have wide-ranging plans to address those challenges. We are never going to have a perfect health system. such a thing does not exist anywhere in Australia, or anywhere in the world. What we do have is a holistic plan through the ACT Health Services Plan released last year and now a 10-year Health Workforce Strategy to address the challenges we already know that we face…
“My work is to get on and implement those strategies and those plans to address the challenges that we know exist.”
Liberals will take Royal Commission to the election
“To dismiss [the call for the Royal Commission] and to say ‘No, no, we’re not going to do this because we’ve got all the answers’ is absolute rubbish,” Mr Hanson said.
“It’s letting down the staff, it’s letting down the patients, and it is not credible. If we’ve got all the answers, as the government says, why is it the worst performing health system in Australia? …
“What we’ve seen from this government is a tendency, wherever they can, to hide the detail, defend the indefensible, and put out spot fires …”
Doctors, Mr Hanson said, had told the Liberals that clinicians were leaving the health system because of “continual denials” from the government.
“The doctors and the nurses know there’s a real problem, and when they hear from the minister ‘Everything’s OK, we’ve got it all in hand’, when they don’t, it’s very frustrating.
“What staff in the hospital want to know is that there’s an acknowledgement there is a problem, there’s a whole range of problems, and there is a plan to fix it. For the government to say that they know all the problems and they are fixing all the problems, the evidence does not bear that out.”
Mr Hanson said that a hospital clinician rang him today to thank him for the Royal Commission proposal. However, Mr Hanson continued, the clinician would not give their name.
“I can’t possibly say who I am because of the nature of this government – what would happen to me?” the clinician reportedly said.
On the financial front, Mr Hanson argued that in the context of the ACT Budget, the Royal Commission was “a small amount of money to provide a big fix”. Health was the most important system in the ACT, costing $2.2 billion every year, or $9 billion over a four-year term of government; it employed thousands of staff and engaged with tens of thousands of patients every year.
Mr Hanson noted that while the minister “doesn’t want to do a review”, Ms Stephen-Smith had spent $1.5 million on rebranding Canberra Health Services (including two new roles and an $800,000 two-year contract with a design company).
- Canberra Health Services rebrand: marketing or makeover? (21 February 2023)
Mr Hanson thought that the Royal Commission would take a year to 18 months. It need not report until after the next election.
“We want to take this out of the political cycle,” Mr Hanson said. “We don’t want this to be a political issue. What we want is a fix to the health system. It’s quite clear that whilst the government is putting out the very many spot fires in health, what they don’t have is the sort of strategic vision and plan that they need – and, quite frankly, we would need, should we form government. This is about fixing a broken system.”
If the ACT Government rejects the Liberals’ motion next week, Mr Hanson promised, the opposition will take it as a commitment to next year’s election.
The Liberals will also present a suite of policies in health (including infrastructure, staffing, and fixing problems in the emergency department).